Osteoporosis Part 2:
How to build stronger bones through exercise
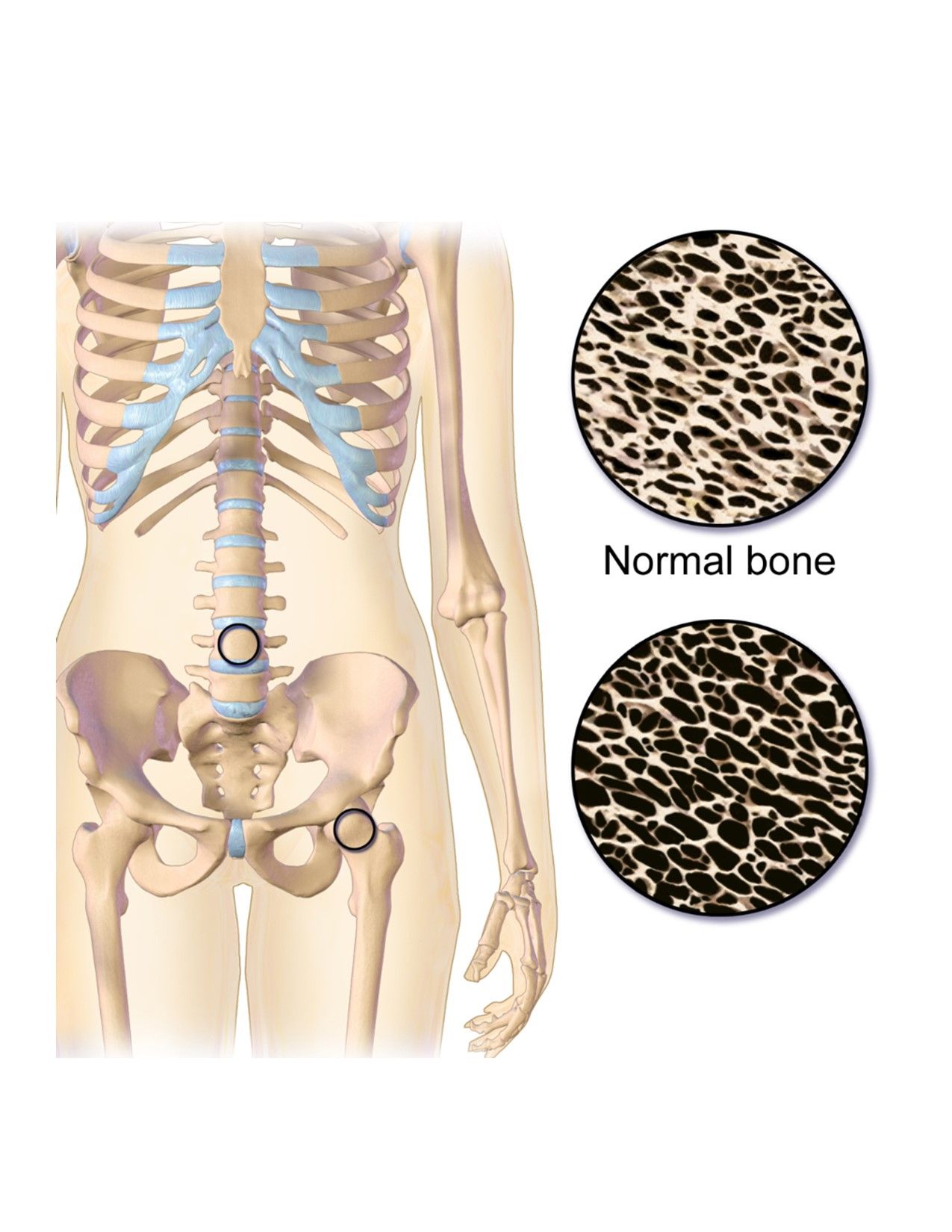
If you missed my first article on osteoporosis (OP), make sure to go back and check it out! That article explains what osteoporosis is, and who is more at risk for being diagnosed with OP. This article will focus more on the evidence behind building stronger bones with exercise, and thus lessening the effects of osteoporosis. Of course there are also a lot of nutritional recommendations for OP, but that is beyond our scope of practice. Please consult your doctor or dietitian for more information on how nutrition can help OP!
What types of exercise are best to improve my bone strength (aka bone mineral density - BMD) if I have osteoporosis?
Basically, a combination of exercise is best. We know for sure that weight-bearing (WB) exercises help build bone density, which means any type of exercise that is putting weight through your bones. So for your legs and spine, this would be any upright/standing exercises. For your arms and upper trunk, this would be anything that puts weight through your arms like planks or push-ups (yes, even the version on the wall!).
The cool thing is that we also see these improvements in BMD with any type of resistance exercise: free weights, dumbbells, resistance bands, etc. The sky is the limit! And of course, we know generally that people with OP are at a higher risk for falls and broken bones as a result of those falls. So including some balance training and aerobic exercises are recommended as well.
How often do I need to exercise to see improvements in my bone health?
Studies indicate that to achieve an increase in bone mineral density, the frequency of training should be 2–3 times per week for 30–60 minutes, depending on the intensity. Twelve weeks’ duration is the minimum to see increases in BMD.
Is there any research showing the benefits of certain types of exercise?
Absolutely! Here’s a short list:
- Aerobic weight-bearing exercises: walking, stair climbing, jogging, dancing, and Tai Chi have all been shown to be beneficial for bone health (note: walking alone isn’t enough to improve BMD unless paired with another type of exercise!)
- Resistance training: especially focused on the glutes, lower back, and upper body
- Hi-intensity resistance and impact training (HiRIT): HiRIT has the potential to be better at improving bone density as it is more intense than low-impact exercise, and has been shown to be safe in postmenopausal people with vulvas who have osteopenia and osteoporosis
- Balance/coordination exercises: can reduce fall risk and thus fracture risk
- Whole-body vibration: this is a therapy intervention in which the whole body is vibrated to activate mechanoreceptors that help improve bone growth
- Aquatic therapy (exercise in a pool): exercise in the pool is often tolerated better by older adult patients, plus a review found that it can be successful in maintaining BMD
This is all so fascinating! So how can physical therapy help?
A physical therapist (PT) can help make an individualized exercise program for you. This will take into account the location(s) in which you have OP, and any associated muscle weaknesses or tightness that need to be addressed. Plus, a PT can also help you “dose” your exercise appropriately - finding that “just right” amount between too little and too much. And then of course, your PT can also give you exercises to either relieve any current pain that you have, or prevent you from developing pain later on!
References:
Dressendorfer, R, BscPT, PhD, and A, MPT Callanen. “Osteoporosis and Exercise.” CINAHL Rehabilitation Guide, edited by DhSc, MSPT, PT Richman S, Aug. 2021. EBSCOhost, https://search.ebscohost.com/login.aspx?direct=true&db=rrc&AN=T709163&site=eds-live
National Institutes of Health (NIH) page on osteoporosis diagnosis, treatment, and steps to take:
https://www.niams.nih.gov/health-topics/osteoporosis/diagnosis-treatment-and-steps-to-take